One of my best cases was 29 year old was dropped off at the ER all burned over his thighs, legs, arms and belly. He stated he "woke up and was on fire." So we are in the ambulance with him in the back. He has already been intubated, as we must do with all burns over 40% of your body to prevent lung collapse (this is a long explaination just trust me on that) so he is unconscious. When we get to the big hospital, they route us to the wash out bay. Apparently, since the fire is of unknown origin and obviously suspicious they are going with meth lab explosion. Since that kind of a burn would involve various caustic chemicals that could burn hospital staff it means we must go through decontamination protocol and wash him off with a certain amount of water before they will bring him in the building. Unfortunately, this guy has been crashing in the ambulance, with irregular heart beats and the heart monitor is not something that works well when sprayed with water.

Despite our attempts to fix it, they took off his monitor for 3 minutes to wash him down. Luckily, nothing unseemly happened and the doc got in to see him right away. It was quickly determined these burns were not from a meth lab explosion but rather from electricity. The muscle in man's leg was rock hard under those horrible burns. It was something I've never seen in real life until today, but something med school always warns us about: Compartment Syndrome. The muscles and skin in his body were so inflamed from having electric bolts running through them, that they were expanding and filling his thighs to the point where they choked off his arteries and nerves. He can lose body parts and eventually have his heart give out because of this. The doctor took out a big knife and cut a long, deep cut down to the muscle from pelvis to knee on both sides, his pink muscles squeezed out of the cuts like toothpaste. Then he did his arms, lucky this guy wasn't awake. Apparently, he had been stealing copper wire from a live set of wires on a power line. And of course got burned. He ended up having several of his fingers amputated because the flesh and muscle were so burned they would never be functional again. This is a picture of his hand. I didn't get the best shot, which was his palm because the docs didn't want me to take pictures because of his critical condition.
Beyond that case, I did get to participate in a Code Grey or a Mass Casualty. We had a huge 10+ car pile up including a bus full of kids. So we called in all our docs and had people being checked over in hallways, closets, and 3 people per room. We had crazy parents running all over the place and causing a rukus, which didn't help anything and in the meantime we had several seriously injured adult patients from the same crash. It was amazingly chaotic, just the way I like it!
We also had a inner hospital tradgedy. A 28yo internal med resident who went down to the ER on her shift and checked in as a patient because she had such a huge headache. And 6 hours later, she was dead. Meningitis. It was intense. Everyone around the hospital that day was crying and calling in to see if they could get antibiotic prophylaxis. Then her parents came and everything in the hospital stopped because everyone wanted to talk to them, docs, nurses, even some patients for whom she had made a difference. It was just so close to home, I think it really made a lot of people think hard about their choices.
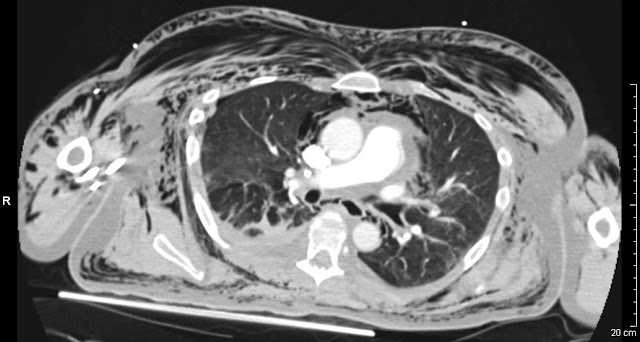
The final crazy story I have from this rotation was a 15yo boy who came in after playing paintball. He had taken off his helmet to wipe the fog from the visor, when a paintball nailed him in the eye. When I saw it was swollen to the point where it couldn't open even when i tried to pry it open. THe poor kid was in shock I think, because he didn't really know what was happening. We got a CT scan to see what was going on and we noticed that the normal bulge of the eye wasn't there. And sure enough, the eyeball had ruptured, we call it a globe rupture. There is very little likelihood that he will ever be able to see out if it again. They took him to surgery to see if they could save it. This case was especially memorable for me, because I had to tell the parents what happened and that their son would most likely not have 2 eyes. Last I heard, the surgeons were discussing glass eyes with the parents.